The Human Side of Medicaid Work Requirements
Four priorities for leaders to meet federal rules without losing sight of residents

As states prepare to implement H.R. 1 Medicaid work requirements, much of the focus has been on defining policy and building systems for data matching. Verifying compliance through data matching is the best-case scenario to reduce the burden of these requirements on residents, but it won’t be enough on its own.
Even if data matching worked for every eligible person, millions of residents across the country will still need to take action or risk losing coverage for procedural reasons. If states underestimate the communication and design challenge in H.R. 1 implementation, residents will miss deadlines, eligibility staff and call centers will be overwhelmed, and public trust in safety net programs will erode further. User experience will be central to whether eligible people keep coverage and whether staff can manage the workload.
Christil, a mother of two Civilla met during our research, knows what’s at stake. During the week, she stays home with her children while her husband works full-time. On weekends, they switch roles so she can earn a paycheck. Their schedules are already stretched thin. When she learned about work requirements, her worry wasn’t about working 80 hours. It was about the added paperwork.
“My husband and I already never see each other. How much more time do we have to give up to meet these requirements?”
Her question points to the heart of implementation: not just bringing programs into compliance, but determining how people will experience them. Based on Civilla’s work with residents and state agencies, four priorities stand out for leaders.
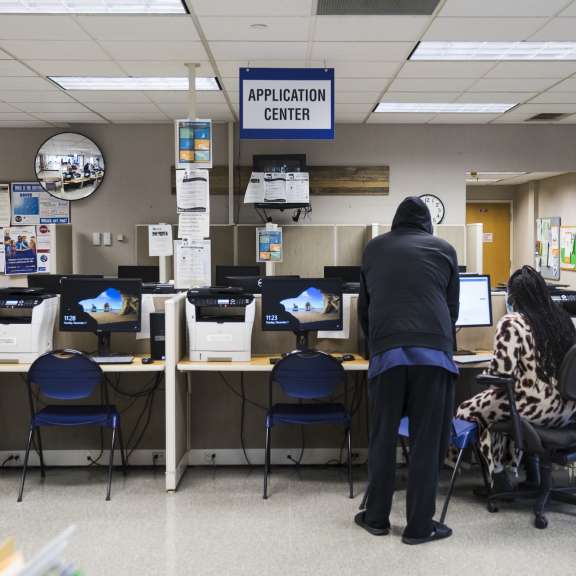
1. Start with applications
The application is the first place many residents will encounter the new rules. If the process is confusing or fragmented, people will fall off before they ever establish coverage. States should integrate exemption screening and work activity questions directly into a single streamlined application on paper and online, rather than creating a separate follow-up step.
A clearly labeled section helps residents know where to look. Begin by screening for exemptions with simple yes/no questions, then route only those who need to report hours into a short work-activity grid. In online forms, conditional logic can keep people from answering irrelevant questions. Taken together, these steps will make the process more straightforward for residents and create a cleaner pipeline for state systems to verify compliance.
2. Design clear correspondence
Residents will need education before the requirements take effect. Letters and notices will determine whether residents take action or miss deadlines. Outreach should begin well in advance, with repeated communication through notices, texts, and portal notifications. These messages should explain what is changing, what it means for a person’s case, and what action is required. Without clear communication, residents will flood call centers and offices in search of answers, overwhelming already stretched staff.
States will need to avoid burying the lede in dense, technical language. Terms like “exemption” and “qualifying activity” are not part of most people’s vocabulary. If residents don’t understand what is being asked, they can’t comply. Clear correspondence can save caseworkers thousands of hours and reduce unnecessary churn.

3. Use text communications strategically
Letters alone won’t reach people in time. Text messages are an essential complement for reminders about reporting and exemptions. Residents told us that the right message—short, urgent, and actionable—would prompt them to act immediately. The wrong one, packed with jargon or no clear calls to action, would get ignored.
Texts should mirror the clarity of redesigned correspondence: one action, one deadline, one link. Leading with phrases like “Action Needed” will build urgency. States should build smart notification systems that send reminders tied to key dates, easing the load on staff while helping residents stay compliant.
4. Design digital flows that set people up for success
Many residents will be required to report hours or claim exemptions online, making digital design a critical part of setting people up for success. Mobile-friendly, step-by-step flows that use plain language will reduce errors and drop-offs. Systems that mirror legal code or combine multiple tasks on a single screen will create confusion. Leaders should insist that digital tools be designed from the resident’s perspective, not just to meet policy requirements.
researched guidance for states
Christil’s story reminds us that benefit recipients are already navigating complex lives. How states design these requirements will decide whether people like her can keep coverage or fall through the cracks.
To support leaders in this work, Civilla has released a new report on human-centered Medicaid work requirements. Drawing on research conducted in Michigan, the report shares practical, user-tested recommendations that show how states can meet federal rules while reducing administrative burden, protecting coverage, and strengthening trust